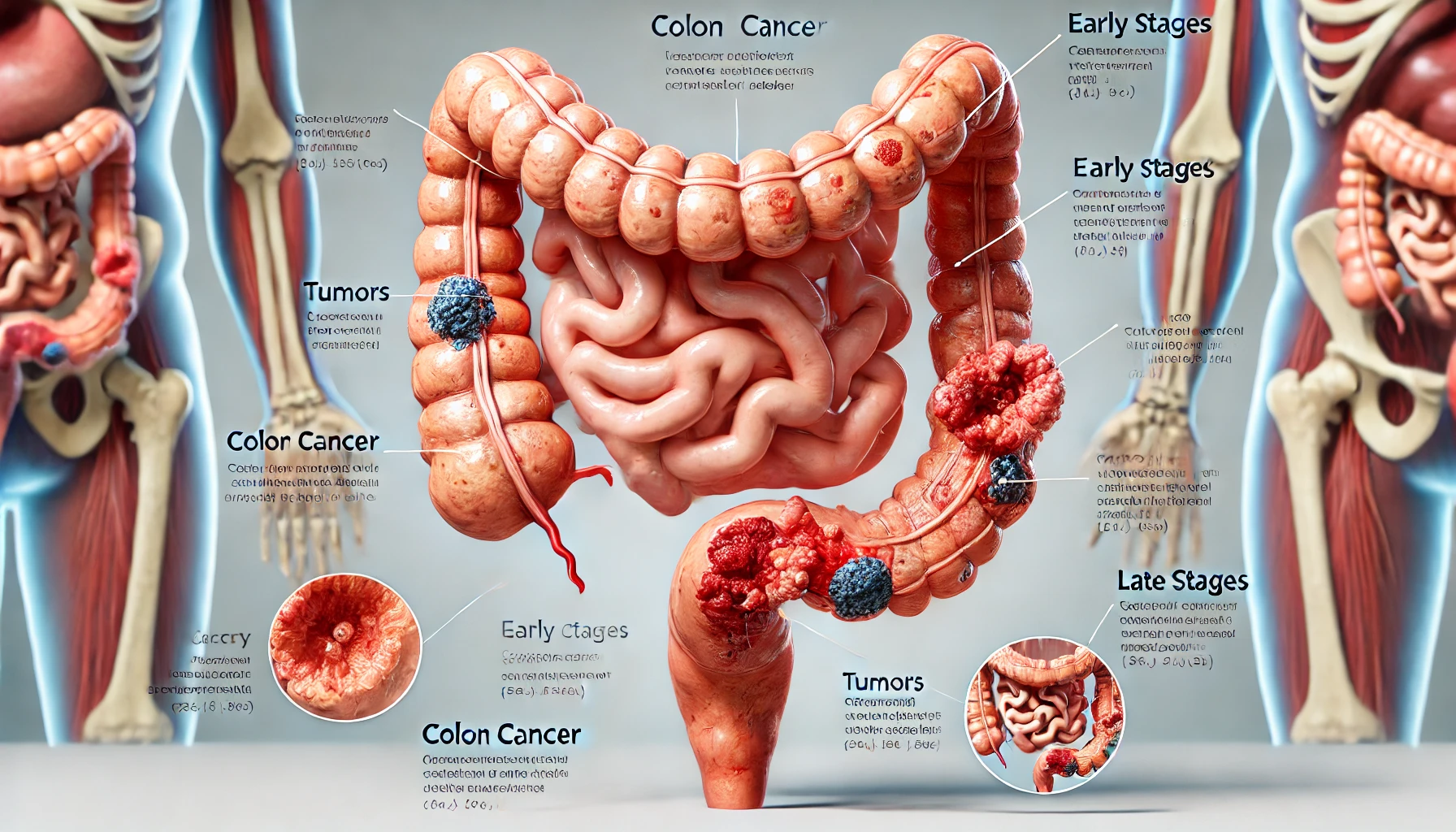
Colon Cancer?
Colon cancer, also known as colorectal cancer, is one of the most common types of cancer affecting millions of people worldwide. However, it is also one of the most preventable forms of cancer. According to the World Health organization (WHO), colorectal cancer ranks as the third most common cancer globally, and it’s the second-leading cause of cancer deaths. In the United States alone, the American Cancer Society reports that over 150,000 people will be diagnosed with colorectal cancer each year, and around 52,000 will lose their lives to the disease. These statistics reveal the urgent need for awareness and prevention.
Early screening and lifestyle modifications can frequently avoid colon cancer. Despite its gravity, a lot of individuals are still ignorant of the doable precautions they can take. The purpose of this blog is to explain the facts, the dangers, and easy yet efficient steps you may take to lower your risk of colon cancer.
Risk Factors
Several risk factors can increase the likelihood of developing colon cancer, including numerous environmental, lifestyle, and genetic variables are risk factors for colon cancer. Here are a few important ones:
- Age: Most cases of colon cancer are diagnosed in people over 50, though it can occur in younger individuals as well.
- Family History: An increased risk may result from a family history of colon cancer or polyps.such as Lynch syndrome or familial adenomatous polyposis (FAP), increases risk
- Obesity: A higher risk of colon cancer is associated with being overweight or obese.
- Physical Inactivity: Living a sedentary life can increase your risk.
- Alcohol and Smoking: Excessive alcohol use and smoking are linked to an increased risk of colon cancer.
- Diet: Diets high in red and processed meats, low fiber, and low intake of fruits and vegetables have been associated with increased colon cancer risk.
- Type 2 Diabetes: Individuals with type 2 diabetes are at a slightly higher risk.
Modifications to Lifestyle for Prevention
The risk of colon cancer can be considerably decreased by adopting specific lifestyle modifications. Here are a few successful tactics:
Sustain a Healthy Weight
One known risk factor for colon cancer is obesity. This risk can be reduced by maintaining a healthy weight through regular exercise and a balanced diet. Get at least 150 minutes of moderate-intensity activity per week and strive for a body mass index (BMI) that is within the normal range.
Maintain a Balanced Diet
The risk of colon cancer can be decreased by eating a diet high in fruits, vegetables, whole grains, and lean proteins. Take into account the following dietary advice:
- Increase Fiber Intake: High-fiber foods, such as beans, lentils, whole grains, fruits, and vegetables, can help promote healthy digestion and reduce the risk of polyps.
- Limit Red and Processed Meats: Reducing consumption of red meat and avoiding processed meats can lower cancer risk.
- Incorporate Healthy Fats: Opt for healthy fats, such as those found in avocados, nuts, and olive oil, while limiting saturated and trans fats.
- Fruits and veggies: Try to have a range of fruits and veggies on half of your plate. These are high in fibre, vitamins, and minerals. To receive a variety of nutrients, choose colourful foods like tomatoes, carrots, leafy greens, and berries.
- Whole Grains: Opt for whole grains like oats, brown rice, quinoa, and whole-grain bread instead of refined grains. Whole grains provide more fiber and help maintain steady blood sugar levels.
- Lean Protein: Opt for lean protein sources such as poultry, fish, and plant-based proteins (tofu, lentils, and beans). Omega-3 fatty acids, which have anti-inflammatory qualities, are found in fish, particularly fatty fish like salmon.
- Healthy Fats: Choose healthy fats from foods like avocados, nuts, seeds, and olive oil. Compared to rich or fried foods, these fats are easier on the digestive tract and help lower inflammation.
- Hydration: Drink water, herbal teas, and broths to be well hydrated. Maintaining adequate water keeps the digestive tract in good working order and aids in the efficient action of fibre.
- Fermented Foods: Yoghurt, kefir, sauerkraut, kimchi, and other foods high in probiotics might help maintain a balanced gut microbiota, which may be good for colon health.
- Green Tea: Polyphenols, which are abundant in green tea, have antioxidant qualities and may help prevent cancer. Including one or two cups daily in your diet can be beneficial.
This diet can lower the risk of colon cancer and promote general health when paired with routine exercise and checkups. For individualised guidance, always seek the advice of a medical professional or dietitian, particularly during or following treatment.
Why Routine Screening Is Important
Regular screenings are vital for early detection and prevention of colon cancer. The American Cancer Society recommends that individuals at average risk begin screening at age 45. Those with a family history or other risk factors may need to start earlier. Screening options include:
Colonoscopy
A procedure that allows doctors to examine the entire colon and remove polyps if necessary. It is recommended every 10 years for those at average risk.
Flexible Sigmoidoscopy
Similar to a colonoscopy but examines only the lower part of the colon. It is recommended every five years.A medical treatment called a flexible sigmoidoscopy is performed to look at the rectum and sigmoid colon, which are located in the lowest portion of the colon. To check into the colon and find any anomalies like polyps, inflammation, or cancer, a doctor performs this operation using a sigmoidoscope, a thin, flexible tube with a light and camera on the end.
Stool Tests:
Stool tests are non-invasive medical procedures used to diagnose a variety of digestive system disorders by analysing a sample of stool, or faeces. They are frequently employed to find indications of colorectal cancer, infections, and digestive problems. A closer look at the types, methods, and objectives of stool tests is provided below:
- Detect gastrointestinal infections (such as those caused by bacteria, viruses, or parasites).
- Diagnose digestive issues like malabsorption, inflammatory bowel disease (IBD), and irritable bowel syndrome (IBS).
- Screen for colorectal cancer by detecting hidden (occult) blood in the stool.
- Fecal Occult Blood Test (FOBT): This test checks for hidden blood in the stool, which can be a sign of colorectal cancer or polyps
Family history and genetic testing
Genetic testing can be a possibility for people who have a family history of colon cancer. The risk of colon cancer can be considerably raised by specific genetic abnormalities, such as those linked to Lynch syndrome or familial adenomatous polyposis (FAP). Consult your healthcare practitioner about genetic testing if colon cancer runs in your family.
Conclusion
A multimodal strategy including dietary adjustments, lifestyle changes, and routine screenings is needed to prevent colon cancer. People can greatly lower their risk by eating a balanced diet, remaining physically active, avoiding tobacco and excessive drinking, and maintaining a healthy weight. Regular screenings are also essential for prevention and early detection. To create a customised preventative strategy, speak with your healthcare professional if you have a family history of colon cancer or other risk factors.
People can lower their risk of colon cancer and empower themselves to live healthier lives by being proactive in their prevention. Keep in mind that making educated decisions now can result in a healthy tomorrow and that early detection saves lives.
Disclaimer
The Content provided here is for informational purpose only. This Blog is not intended to substitute for medical advice , diagnosis , or treatment. Always seek the advice of a qualified healthcare provider for any questions or concerns you may have regarding a medical condition. Writerspirit does not endorse or recommend any specific tests, physician , procedures ,opinion , or other information mentioned on the blog.
FAQs
What is colon cancer?
Colorectal cancer, another name for colon cancer, starts in the colon or rectum, which are sections of the large intestine. Usually benign polyps at first, they have the potential to develop into cancer over time.
What causes colon cancer?
Mutations in the DNA of colon cells are the cause of colon cancer. Age (over 50), family history, specific genetic syndromes, lifestyle choices (such as a poor diet and inactivity), obesity, smoking, and excessive alcohol consumption are risk factors.
What are the symptoms of colon cancer?
Symptoms of early-stage colon cancer might not be apparent, but as it advances, they may include:
Constant cramping or pain in the abdomen
1)Alterations in bowel habits, such as constipation or diarrhoea
2)Stool containing blood
3)Unaccounted-for weight loss
4)Weakness or fatigue
How is colon cancer diagnosed?
Common diagnostic tools include:
Colonoscopy: A scope examines the colon for polyps or cancer.
Flexible Sigmoidoscopy: Examines the lower part of the colon.
CT Colonography: Uses CT imaging to visualize the colon.
Stool Tests: Detects blood or abnormal DNA in stool samples.
Who is at risk for colon cancer?
Although risk rises with age, especially after the age of fifty, people who have a family history or genetic abnormalities (such Lynch syndrome) are more vulnerable. Risk can also be raised by lifestyle choices like smoking, drinking alcohol, being obese, and eating poorly.
How can I reduce my risk of colon cancer?
Diet: Eat a balanced diet rich in fiber, fruits, and vegetables.
Exercise: Engage in regular physical activity.
Avoid Smoking and Limit Alcohol: Both can increase risk.
Screening: Regular screening (starting at age 45-50) is one of the most effective ways to detect colon cancer early.
What are the treatment options for colon cancer?
Treatment options depend on the stage and include:
Surgery: Removes cancerous sections of the colon.
Chemotherapy: Uses drugs to kill cancer cells, often after surgery.
Radiation Therapy: Targets cancer cells with high-energy rays.
Targeted Therapy: Targets specific mutations in cancer cells.